Coping with Severe Asthma
Current prednisolone dose: 25mg
Current weight: 321.4lbs (-4.4lbs)
Slightly late this week posting as I’ve been knocked out for a few days with a cold that immediately started to irritate my chest! While I’ve been lying around feeling rough and attempting to tweak things to avoid upping my steroids again/stay out of hospital it got me thinking about how I cope with my asthma - something I’m often asked by friends and family (spoiler alert: I don’t!).
So, without further ado here are my personal tips that I’ve found help me cope with severe, unruly asthma! (Although most of these can be applied to all asthma!)
1. Have an action plan and know it well
This really is so important! Every asthmatic, regardless of how mild or severe should have an action plan in place. It gives a guide on what symptoms to look out for, how you can increase your own medication (for example, increasing your preventer dose) at home and when you should seek further attention (either through your GP or attending hospital). This is often split into peak flow "zones" based on your personal best peak flow (or your predicted if you are newly diagnosed and don't know your best yet).
Generally being in the "amber" zone means you need to increase medication in some way and might need some steroid tablets from your GP and being in the "red" zone tends to mean you need to be heading to hospital! If you struggle to remember the right numbers or can't work them out when you're unwell it might be worth colouring in the side of your peak flow meter - giving a really easy way for you and healthcare staff to see where you are!
2. Keep an eye on your peak flow
Not every asthmatic needs to religiously monitor their peak flow every day. I currently do because I'm still pretty unstable and keeping a close eye means I can sometimes start to pick up a deterioration before I show noticeable symptoms (I spent a great deal of 2018 stuck in the lower amber zone of my peak flow so don't always pay attention to symptoms when I'm there again!).
However, its still important to be aware of your peak flow, and particularly try to find out your personal best. It isn't the exact number that is important but how it compares to your normal - for example, some people will have a lower than expected peak flow and some will have one much higher than expected (especially those who play wind instruments and sing!).
In the past, before my asthma was severe I would start to monitor my peak flow when I got symptoms - for example, if I started waking up coughing in the night I would keep a close eye on it for the next few days to see if it would resolve itself or if I needed to head to the GP.
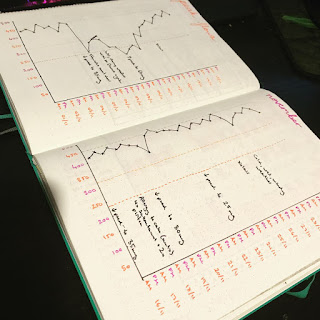
If, like me, you enjoy graphs etc you can keep track of your daily peak flows - I note mine down in my journal and add notes if I've come into contact with any triggers that caused a drop.
3. Don't just rely on your peak flow!
Having talked about the importance of peak flow, its equally important to not only rely on your peak flow! It isn't always a reliable indicator in every asthmatic (it can be very technique and effort dependent for example) and in those who have a much higher than predicted best, can be misinterpreted by medical staff - a peak flow of 300 might be excellent for a lot of asthmatics, but for someone with a personal best of 600 its in the red zone.
How you feel overall is much more important, for example your peak flow might only be in your amber zone, but if you're struggling to get around the house or speak without getting very short of breath something is wrong!
4. Have a way of communicating your history when you can’t speak
Particularly important for any "frequent flyers" to A&E and hospital! When I have a severe attack I'm often unable to speak more than a couple of syllables without needing a break and getting your history across, with number of admissions, any triggers and the medication list can take a veryyyyy long time one word at a time!
So I always make sure I have my "asthma bible" with me - its just a small folder with print outs in covering my medical history, medications and action plan. I also have a medic alert necklace (listing severe asthma, the fact that I'm steroid dependent and my allergies) and discovered that the health app on iphones has sections for your medical history too!
This is often really appreciated by healthcare professionals as it gives them all the information they need quickly and easily, so they can get on with treatment without waiting for me to gasp out medications.
If I get stuck without any of this on me, pen and paper is really useful to communicate and don't be afraid to ask for some if you're really struggling to speak.
5. Keep your GP/asthma team up to date
Fairly self-explanatory and I appreciate this isn't always possible! But I always try to make sure I ring up my asthma nurses if I'm admitted and update them on any flares I've had that I've managed to control at home when I go for my xolair injections every couple of weeks.
I also try to keep my GP up to date with all my repeat prescriptions (as they often change!) and what my current maintenance dose of steroids is.
6. Know your limits/listen to your body
Easier said than done! I'm particularly bad for not always following this one. But its important to remember that an asthma attack is a very tiring experience for your body and recovery can take a long time!
It can be really frustrating when you're recovering if you feel it isn't happening fast enough but it is important to take your time and let yourself rest a bit - if you've had an attack you're more at risk for another in the 2 weeks afterwards so always be careful in this period! I had so many admissions in the past where I would try and immediately return to normal activities afterwards and surprise, surprise I would often end up being readmitted pretty soon after!
7. Have a "grab and go" bag
Another one for the "frequent flyers"! I always make sure I have a little bag stashed somewhere in my room that has some mini toiletries, a couple of pairs of pants, a spare top and a few days worth of my medications in so that if I have to call an ambulance to my house I'm ready to go (my history now means that I almost invariably end up admitted at least for observation and struggle to escape from A&E!).
My little melon bag has my toiletries in and always comes on a hospital trip!
8. Sleep propped up if you’re struggling
I often find that I struggle to sleep when my asthma flares up, particularly if I'm lying flat. So when this happens I grab all my spare pillows and sleep propped up - this helps your lungs to fully inflate while you're asleep and hopefully makes sleeping easier!
9. Have a distraction ready in case of an attack
Every hates being told to "stay calm" and "focus on your breathing" - it never helps people calm down! BUT getting stressed or panicked can make an asthma attack much worse.
So if I start to experience symptoms, especially at night, I'll often put on some music, read a book or try to play a game for a little bit as it helps distract me from the chest tightness and gives my inhalers time to take effect.
10. Have a spare reliever inhaler in your bag
If, like me, you always forget where you've put your inhaler or often swap bags it can be useful to make sure you have a spare one somewhere. This can either be at home in case you lose your main one or in a bag you regularly use (for example I keep one in my handbag) so you don't have to specifically remember to move one into that bag.
11. Work out your triggers and try to avoid them
Sometimes this is easier said than done! But you can still take steps to minimise exposure to your triggers, for example - if you are allergic to pollen and find this sets you off then make sure you take antihistamines during the pollen season.
Another example is the cold weather, and this is particularly hard to avoid as you can't stay in bed every time the temperature drops! But wrapping up warm and wearing a scarf around your mouth when you go outside can help reduce the effect it has on you!
Asthma UK has lots of great info on all the different triggers for asthma and tips for avoiding them/reducing exposure!
https://www.asthma.org.uk/advice/triggers/
12. Don’t be afraid of going to hospital
A lot of people don't like going to hospital (understandably!) - its a scary place and admitting that you're unwell enough to need inpatient treatment can be very stressful. Also people may have been to ITU before which can be a very traumatic experience or had a bad experience with the treatment they've received (a lot of people often feel they're not taken seriously if they don't present with very typical symptoms!).
But if you're really getting to that point its important to not delay seeking further help! Hospital staff would much rather see you early on when it might only take a nebuliser or two to help settle things than a couple of days later when you might need IV medication and a much longer admission to stabilise things! I once put off seeking help far too late and it resulted in me spending 2 weeks on HDU (high dependency unit - in between normal wards and intensive care) and was very nearly intubated a couple of times - its really not worth it for those extra days at home!
If you're stuck on the borderline and are not quite sure if you're bad enough to head in to hospital then try to see your GP (generally mentioning breathing problems on the phone tends to get you a same day appointment) and they can make that decision for you.
13. Find people to talk to/vent
This is so, so important. Asthma, and in fact any chronic illness, can be incredibly stressful and mentally draining. Its really important to have a way of dealing with this, and often having someone to talk to (or rant to!) can really help. There are lots of support communities around online where you can talk to people who understand what its like to deal with asthma and family and friends can often help with this too.
If you really start to feel you are struggling with your mood then its really important to see your GP - depression and anxiety are very common in chronic illness and are completely understandable given the situation!
14. Don’t put your life on hold because of asthma
If you're having a rough time with asthma its very easy to start avoiding activities for fear of causing an attack. But its really important to try to not do this!
Aside from the fact that staying home and not going out can be incredibly isolating (which doesn't help with mood issues), but reducing activity levels means that your physical reserve and strength decreases - meaning you can't cope as well with any further attacks.
15. Take your meds!
I put this last because it is arguably the most important and I wanted it to stand out. Taking medications isn't fun and its not always easy to remember but its so important to make sure you take them as prescribed, as they're designed to try and stop an asthma attack happening in the first place!
Also, don't stop any medications without getting advice - there's nothing wrong with wanting to reduce medication when you're well or stop ones that aren't helping but its important to make sure you consult a healthcare professional first and do it under their guidance.
Current weight: 321.4lbs (-4.4lbs)
Slightly late this week posting as I’ve been knocked out for a few days with a cold that immediately started to irritate my chest! While I’ve been lying around feeling rough and attempting to tweak things to avoid upping my steroids again/stay out of hospital it got me thinking about how I cope with my asthma - something I’m often asked by friends and family (spoiler alert: I don’t!).
So, without further ado here are my personal tips that I’ve found help me cope with severe, unruly asthma! (Although most of these can be applied to all asthma!)
1. Have an action plan and know it well
This really is so important! Every asthmatic, regardless of how mild or severe should have an action plan in place. It gives a guide on what symptoms to look out for, how you can increase your own medication (for example, increasing your preventer dose) at home and when you should seek further attention (either through your GP or attending hospital). This is often split into peak flow "zones" based on your personal best peak flow (or your predicted if you are newly diagnosed and don't know your best yet).
Generally being in the "amber" zone means you need to increase medication in some way and might need some steroid tablets from your GP and being in the "red" zone tends to mean you need to be heading to hospital! If you struggle to remember the right numbers or can't work them out when you're unwell it might be worth colouring in the side of your peak flow meter - giving a really easy way for you and healthcare staff to see where you are!
2. Keep an eye on your peak flow
Not every asthmatic needs to religiously monitor their peak flow every day. I currently do because I'm still pretty unstable and keeping a close eye means I can sometimes start to pick up a deterioration before I show noticeable symptoms (I spent a great deal of 2018 stuck in the lower amber zone of my peak flow so don't always pay attention to symptoms when I'm there again!).
However, its still important to be aware of your peak flow, and particularly try to find out your personal best. It isn't the exact number that is important but how it compares to your normal - for example, some people will have a lower than expected peak flow and some will have one much higher than expected (especially those who play wind instruments and sing!).
In the past, before my asthma was severe I would start to monitor my peak flow when I got symptoms - for example, if I started waking up coughing in the night I would keep a close eye on it for the next few days to see if it would resolve itself or if I needed to head to the GP.
If, like me, you enjoy graphs etc you can keep track of your daily peak flows - I note mine down in my journal and add notes if I've come into contact with any triggers that caused a drop.
3. Don't just rely on your peak flow!
Having talked about the importance of peak flow, its equally important to not only rely on your peak flow! It isn't always a reliable indicator in every asthmatic (it can be very technique and effort dependent for example) and in those who have a much higher than predicted best, can be misinterpreted by medical staff - a peak flow of 300 might be excellent for a lot of asthmatics, but for someone with a personal best of 600 its in the red zone.
How you feel overall is much more important, for example your peak flow might only be in your amber zone, but if you're struggling to get around the house or speak without getting very short of breath something is wrong!
4. Have a way of communicating your history when you can’t speak
Particularly important for any "frequent flyers" to A&E and hospital! When I have a severe attack I'm often unable to speak more than a couple of syllables without needing a break and getting your history across, with number of admissions, any triggers and the medication list can take a veryyyyy long time one word at a time!
So I always make sure I have my "asthma bible" with me - its just a small folder with print outs in covering my medical history, medications and action plan. I also have a medic alert necklace (listing severe asthma, the fact that I'm steroid dependent and my allergies) and discovered that the health app on iphones has sections for your medical history too!
This is often really appreciated by healthcare professionals as it gives them all the information they need quickly and easily, so they can get on with treatment without waiting for me to gasp out medications.
If I get stuck without any of this on me, pen and paper is really useful to communicate and don't be afraid to ask for some if you're really struggling to speak.
5. Keep your GP/asthma team up to date
Fairly self-explanatory and I appreciate this isn't always possible! But I always try to make sure I ring up my asthma nurses if I'm admitted and update them on any flares I've had that I've managed to control at home when I go for my xolair injections every couple of weeks.
I also try to keep my GP up to date with all my repeat prescriptions (as they often change!) and what my current maintenance dose of steroids is.
6. Know your limits/listen to your body
Easier said than done! I'm particularly bad for not always following this one. But its important to remember that an asthma attack is a very tiring experience for your body and recovery can take a long time!
It can be really frustrating when you're recovering if you feel it isn't happening fast enough but it is important to take your time and let yourself rest a bit - if you've had an attack you're more at risk for another in the 2 weeks afterwards so always be careful in this period! I had so many admissions in the past where I would try and immediately return to normal activities afterwards and surprise, surprise I would often end up being readmitted pretty soon after!
7. Have a "grab and go" bag
Another one for the "frequent flyers"! I always make sure I have a little bag stashed somewhere in my room that has some mini toiletries, a couple of pairs of pants, a spare top and a few days worth of my medications in so that if I have to call an ambulance to my house I'm ready to go (my history now means that I almost invariably end up admitted at least for observation and struggle to escape from A&E!).
My little melon bag has my toiletries in and always comes on a hospital trip!
8. Sleep propped up if you’re struggling
I often find that I struggle to sleep when my asthma flares up, particularly if I'm lying flat. So when this happens I grab all my spare pillows and sleep propped up - this helps your lungs to fully inflate while you're asleep and hopefully makes sleeping easier!
9. Have a distraction ready in case of an attack
Every hates being told to "stay calm" and "focus on your breathing" - it never helps people calm down! BUT getting stressed or panicked can make an asthma attack much worse.
So if I start to experience symptoms, especially at night, I'll often put on some music, read a book or try to play a game for a little bit as it helps distract me from the chest tightness and gives my inhalers time to take effect.
10. Have a spare reliever inhaler in your bag
If, like me, you always forget where you've put your inhaler or often swap bags it can be useful to make sure you have a spare one somewhere. This can either be at home in case you lose your main one or in a bag you regularly use (for example I keep one in my handbag) so you don't have to specifically remember to move one into that bag.
11. Work out your triggers and try to avoid them
Sometimes this is easier said than done! But you can still take steps to minimise exposure to your triggers, for example - if you are allergic to pollen and find this sets you off then make sure you take antihistamines during the pollen season.
Another example is the cold weather, and this is particularly hard to avoid as you can't stay in bed every time the temperature drops! But wrapping up warm and wearing a scarf around your mouth when you go outside can help reduce the effect it has on you!
Asthma UK has lots of great info on all the different triggers for asthma and tips for avoiding them/reducing exposure!
https://www.asthma.org.uk/advice/triggers/
12. Don’t be afraid of going to hospital
A lot of people don't like going to hospital (understandably!) - its a scary place and admitting that you're unwell enough to need inpatient treatment can be very stressful. Also people may have been to ITU before which can be a very traumatic experience or had a bad experience with the treatment they've received (a lot of people often feel they're not taken seriously if they don't present with very typical symptoms!).
But if you're really getting to that point its important to not delay seeking further help! Hospital staff would much rather see you early on when it might only take a nebuliser or two to help settle things than a couple of days later when you might need IV medication and a much longer admission to stabilise things! I once put off seeking help far too late and it resulted in me spending 2 weeks on HDU (high dependency unit - in between normal wards and intensive care) and was very nearly intubated a couple of times - its really not worth it for those extra days at home!
If you're stuck on the borderline and are not quite sure if you're bad enough to head in to hospital then try to see your GP (generally mentioning breathing problems on the phone tends to get you a same day appointment) and they can make that decision for you.
13. Find people to talk to/vent
This is so, so important. Asthma, and in fact any chronic illness, can be incredibly stressful and mentally draining. Its really important to have a way of dealing with this, and often having someone to talk to (or rant to!) can really help. There are lots of support communities around online where you can talk to people who understand what its like to deal with asthma and family and friends can often help with this too.
If you really start to feel you are struggling with your mood then its really important to see your GP - depression and anxiety are very common in chronic illness and are completely understandable given the situation!
14. Don’t put your life on hold because of asthma
If you're having a rough time with asthma its very easy to start avoiding activities for fear of causing an attack. But its really important to try to not do this!
Aside from the fact that staying home and not going out can be incredibly isolating (which doesn't help with mood issues), but reducing activity levels means that your physical reserve and strength decreases - meaning you can't cope as well with any further attacks.
15. Take your meds!
I put this last because it is arguably the most important and I wanted it to stand out. Taking medications isn't fun and its not always easy to remember but its so important to make sure you take them as prescribed, as they're designed to try and stop an asthma attack happening in the first place!
Also, don't stop any medications without getting advice - there's nothing wrong with wanting to reduce medication when you're well or stop ones that aren't helping but its important to make sure you consult a healthcare professional first and do it under their guidance.




Comments
Post a Comment